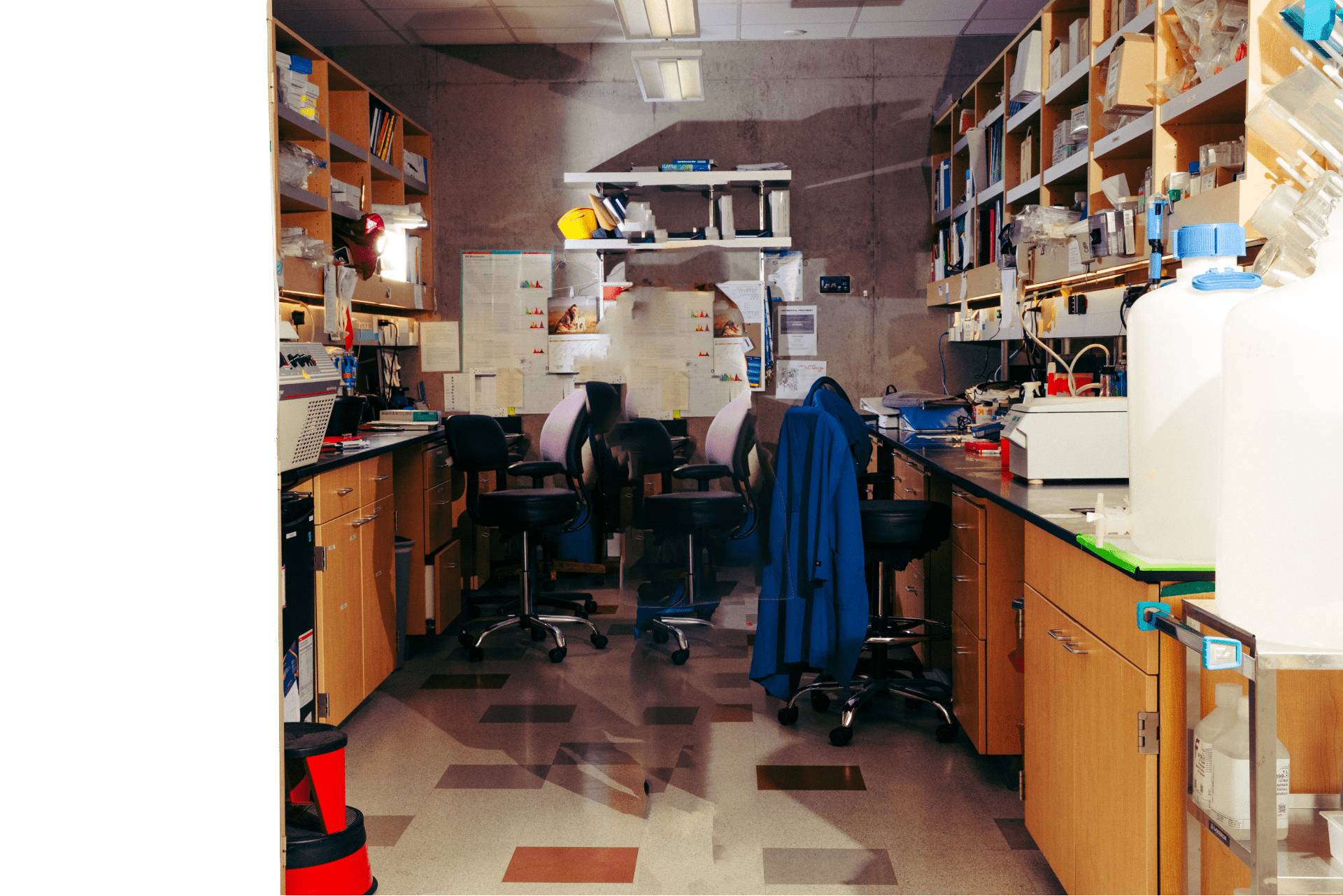
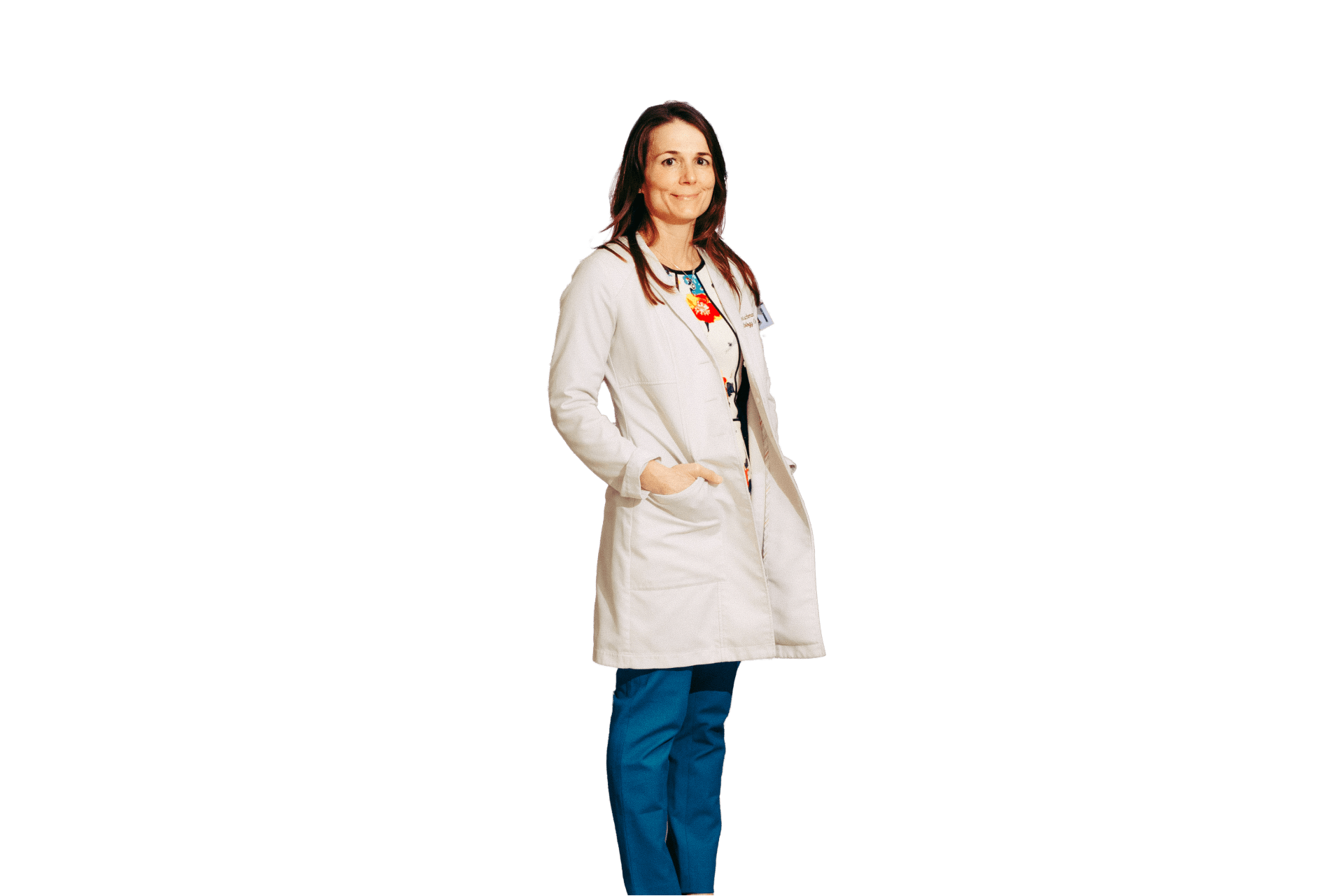
What lies below, says Dr Fleischman, is chronic inflammation. “Inflammation touches everything about MF. It’s not just about the JAK2 clone.” In fact, she questions whether the mutation is a consequence of the disease rather than the source. “In my mind, the bigger issue is why the clone arose in the first place. If you were to somehow get rid of the mutation in a patient with MF, you would still be left with the problem.”
For Dr Fleischman, inflammation is clearly a driver, if not the driver, of MF pathogenesis, and potentially disease progression. When it comes to caring for patients with MF, she urges a more comprehensive approach. “Patients really need more,” she says. “Improving symptoms improves quality of life, and that is important. But patients also need things like blocking the tendency to progress to an acute leukemia, reducing fibrosis, and improving overall survival.”
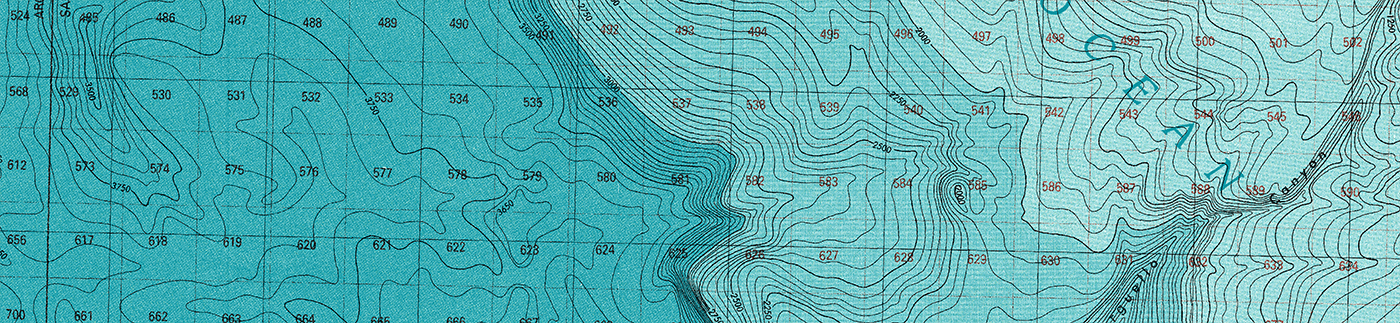
Through her research, Dr Fleischman is helping to make way for a better future for patients with MF by shedding light on the expansive inflammatory landscape that churns the waves of the disease.







.jpg)